1. Putting SARS-CoV2 and COVID-19 in Perspective – the reality of COVID-19 morbidity and recovery
Summary:
Putting COVID-19 in context of:
– other diseases, and
– not taking into consideration inflation of numbers due to misreporting based on ambiguous definitions by the WHO and CDC (see below), in addition to
– potential financial incentives for the reporting of COVID-19 deaths (Miller, 2020),
- COVID-19-related deaths are not any more alarming than any other global disease,
- COVID-19 has a low infection mortality rate and
- The majority of those infected recover from it.
1.1 Definitions in the Age of COVID-19
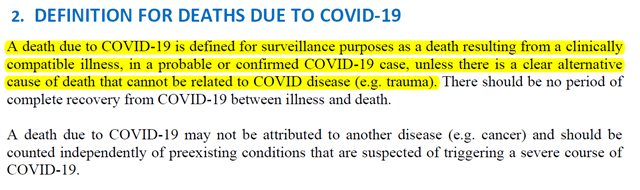
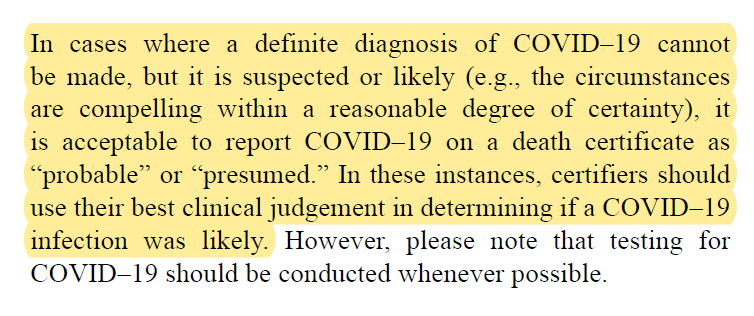
- WHO (WHO, 2020):
- Meddling with definitions is not restricted to deaths by COVID-19 but also in relation to vaccines:
- CDC Definitions of Vaccine and Vaccination (August 26, 2021):
- “Vaccine: A product that stimulates a person’s immune system to produce immunity to a specific disease, protecting the person from that disease. Vaccines are usually administered through needle injections, but can also be administered by mouth or sprayed into the nose.
- Vaccination: The act of introducing a vaccine into the body to produce immunity to a specific disease.”
- “Vaccine: A product that stimulates a person’s immune system to produce immunity to a specific disease, protecting the person from that disease. Vaccines are usually administered through needle injections, but can also be administered by mouth or sprayed into the nose.
- CDC Definitions of Vaccine and Vaccination since September 1, 2021:
- “Vaccine: A preparation that is used to stimulate the body’s immune response against diseases. Vaccines are usually administered through needle injections, but some can be administered by mouth or sprayed into the nose.
- Vaccination: The act of introducing a vaccine into the body to produce protection from a specific disease.”
- “Vaccine: A preparation that is used to stimulate the body’s immune response against diseases. Vaccines are usually administered through needle injections, but some can be administered by mouth or sprayed into the nose.
- CDC Definitions of Vaccine and Vaccination (August 26, 2021):
1.2 False Predictions, Misrepresentation, Intimidation, Terrorizing, Bullying, Labeling & Vilification
- A significant part of the world’s response to COVID-19 was based on faulty models propagated by Dr. Ferguson (Ferguson et al., 2020) from Imperial College, London, whose credibility had already been questioned previously in relation to other models. In an assessment of Dr. Ferguson’s work, Dr. P. Magness, a Senior Research Faculty and Interim Research and Education Director at the American Institute for Economic Research, stated in April 2021:
“So how is the model’s projection performing? Sweden’s government stayed the course with its milder mitigation strategy. As of April 29th, Sweden’s death toll from COVID-19 stands at 2,462, and its hospitals are nowhere near the projected collapse.” - Some models did predict reasonable numbers: “Using variation in demographics, comorbidities and health system capacity, we predict COVID-19 IFRs [infection fatality rate] for 187 countries, ranging from 0.43% in Western Sub-Saharan Africa to 1.45% in Eastern Europe.” (Ghisolfi et al., 2020)
- Two major contributors fueling the COVID-19-related population panic were:
1) the inappropriate categorization of numerous non-COVID-19 related hospitalization cases as a result of vague/ambiguous CDC instructions (National Center for Health Statistics, 2020) in addition to potential financial initiatives (Miller, 2020), and
2) the inappropriate representation of numbers. For numbers to be meaningful, context needs to be provided. Therefore, percentages (in addition to the raw numbers) provide a better understanding of the impact of a disease (e.g., as per schizophrenia, Parkinson’s, etc., when we are referring to prevalence in a population). However, this standard behavior was not followed, and the media, irrespective of ideological allegiance, continued to feed the frenzied panic. The reality of inappropriateness in the use of numbers is indicated in the guidance update of the HHS, issued on January 6, 2022 and effective February 2, 2022 (Health and Human Services, 2022). Under the section “Data Elements Made Inactive for the Federal Data Collection” [emphasis is mine], one of the items listed to be made inactive is the “Previous Day’s COVID-19 Deaths”, which had been the only required reporting of COVID deaths. - A key aspect of this “pandemic” that has been emerging more strongly with time is the intolerance towards those who are critical of the steps taken. This is irrespective of the arguments provided – no scientific or humanitarian fact, no matter how logical, is tolerated. The literature below seeks to address this reality.
- “The present study aimed to investigate whether narcissism levels and message framing strategies affect individuals’ willingness to accept personal restrictions and, consequently, comply with a set of preventive health behaviors. Results reveal that people high (vs. low) in grandiose narcissism are less likely to accept personal restrictions and comply with preventive health behaviors, with negative (vs. positive) message framing constituting a more effective strategy for convincing such individuals to comply with said restrictions and behaviors. This effect can be explained through a more pronounced willingness of participants high in grandiose narcissism to accept personal restrictions to protect themselves (egoistic motivation) but not through a willingness to protect vulnerable people (altruistic motivation). Our findings suggest that individuals who remain uncooperative during pandemics could be more effectively addressed with adapted message framing strategies and incentives tailor-made for their distinct personalities.” (Otterbring et al., 2021) [Interpretation: manipulate the narrative/information and provide incentives; this has been evident for some time, with billboards featuring children, when the minimal vulnerability of children to the virus and the harm of the vaccines to younger ages is clearly documented]
- The National Terrorism Advisory System updated its definition of terrorism on February 7, 2022. In the advisory are addressed key factors “contributing to the current heightened threat environment”. The first factor addressed is:
“(1) The proliferation of false or misleading narratives, which sow discord or undermine public trust in U.S. government institutions:
- For example, there is widespread online proliferation of false or misleading narratives regarding unsubstantiated widespread election fraud and COVID-19. Grievances associated with these themes inspired violent extremist attacks during 2021.” [Interpretation: Truth does not matter. The only “truth” that exists is that provided by the governmental institutions]
- “The present study aimed to investigate whether narcissism levels and message framing strategies affect individuals’ willingness to accept personal restrictions and, consequently, comply with a set of preventive health behaviors. Results reveal that people high (vs. low) in grandiose narcissism are less likely to accept personal restrictions and comply with preventive health behaviors, with negative (vs. positive) message framing constituting a more effective strategy for convincing such individuals to comply with said restrictions and behaviors. This effect can be explained through a more pronounced willingness of participants high in grandiose narcissism to accept personal restrictions to protect themselves (egoistic motivation) but not through a willingness to protect vulnerable people (altruistic motivation). Our findings suggest that individuals who remain uncooperative during pandemics could be more effectively addressed with adapted message framing strategies and incentives tailor-made for their distinct personalities.” (Otterbring et al., 2021) [Interpretation: manipulate the narrative/information and provide incentives; this has been evident for some time, with billboards featuring children, when the minimal vulnerability of children to the virus and the harm of the vaccines to younger ages is clearly documented]
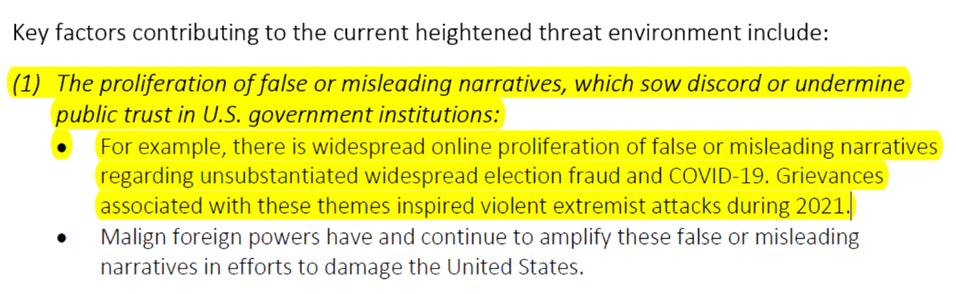
Figure 1: https://www.dhs.gov/ntas/advisory/national-terrorism-advisory-system-bulletin-february-07-2022
- Wang et al. (2022)
- “Excess mortality due to the COVID-19 pandemic, defined as the net difference between the number of deaths during the pandemic (measured by observed or estimated all-cause mortality) and the number of deaths that would be expected on the basis of past trends in all-cause mortality, is therefore a crucial measure of the true toll of the COVID-19 pandemic.”
- “Our estimates of COVID-19 excess mortality suggest the mortality impact from the COVID-19 pandemic has been more devastating than the situation documented by official statistics. Official statistics on reported COVID-19 deaths provide only a partial picture of the true burden of mortality. The difference between excess mortality and reported COVID-19 deaths might be a function of underdiagnosis due to insufficient testing, reporting challenges, or higher than expected mortality from other diseases due to pandemic-related changes in behaviours or reduced access to health care or other essential services” [Interpretation: The study appears to be admitting that there were excess deaths associated with COVID-19, however, contrary to available evidence, blames the deaths on the virus rather than the measures implemented and the negative consequences they caused (e.g., drug overdoses, suicides, ventilator misuse, etc., etc.)]
- “Excess mortality due to the COVID-19 pandemic, defined as the net difference between the number of deaths during the pandemic (measured by observed or estimated all-cause mortality) and the number of deaths that would be expected on the basis of past trends in all-cause mortality, is therefore a crucial measure of the true toll of the COVID-19 pandemic.”
- The confusion and manipulation that exists in regards to the numbers pertaining to COVID-19 deaths is evident at multiple levels:
- Addressed earlier, the HHS stopped the counting of COVID-19 related deaths (Health and Human Services, 2022),
- The CDC has also in discretely placed footnotes indicated that “On August 12, 2021, data on deaths were adjusted after the identification of a data discrepancy. This resulted in updated counts across several age groups. On March 15, 2022, data on deaths were adjusted after resolving a coding logic error. This resulted in decreased death counts across all demographic categories.”
- Addressed earlier, the HHS stopped the counting of COVID-19 related deaths (Health and Human Services, 2022),
Figure 2: footnote from https://covid.cdc.gov/covid-data-tracker/#demographics accessed 03/21/22
- Yet papers continue to argue for increased numbers (e.g., Stokes et al., 2021; Wang et al., 2022), never admitting or considering the biopsychosocial destruction (e.g., increased deaths due to drug overdoses, etc.) that resulted from the measures.
1.3 COVID-19 in Context
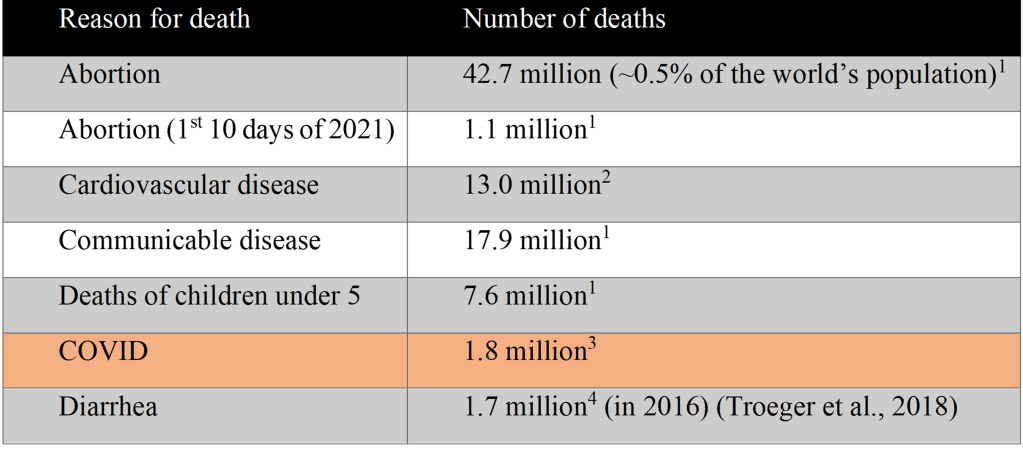
- Global statistics for comparison with COVID-19-related deaths. Unless indicated otherwise, data is for 2020.
Table 1: Comparison of number of deaths associated with various causes
1 https://www.worldometers.info/ (Percentage is calculated from # abortions in 2020/Current World Population)
2 https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1
3 https://coronavirus.jhu.edu/
4 Troeger et al., 2018
- COVID-19 is considered to have a LOW infection mortality rate (IFR) as indicated by the statistics below O’Driscoll et al. (2021) [Data is “age-specific COVID-19-associated death data from 45 countries and the results of 22 seroprevalence studies”]
- COVID-19 Fatality rates by age:
- 0-4 yrs old: 0.003%,
- 5-9 yrs old: 0.001%,
- 10-14 yrs old: 0.001%,
- 15-19 yrs old: 0.003%,
- 20-24 yrs old: 0.006%,
- 25-29 yrs old: 0.013%,
- 30-34 yrs old: 0.024%,
- 35-39 yrs old: 0.040%,
- 40-44 yrs old: 0.075%,
- 45-49 yrs old: 0.121%,
- 50-59 yrs old: 0.323%,
- 60-64 yrs old: 0.456%,
- 65-69 yrs old: 1.075%,
- 70-74 yrs old: 1.674%,
- 75-79 yrs old: 3.203%,
- 80+ yrs old: 8.2%
- Note: An 80 year old has a 6% chance of dying from anything within a year; An 85 year old has a 10% chance.
- COVID-19 Fatality rates by age:
- Other papers that reflect similar information include:
- “Age-specific COVID-19 cases and deaths in Victoria, Australia, during 25 January through 10 December, 2020. Observed case fatality risk (CFR) is the ratio of deaths to cases.” (data in Table 1):
- 0-9 yrs old: 0%; 10-19 yrs old: 0%; 20-29 yrs old: 0.02%; 30-39 yrs old: 0.06%; 40-49 yrs old: 0.04%; 50-59 yrs old: 0.63%; 60-69 yrs old: 2.16%; 70-79 yrs old: 14.41%; 80-89 yrs old: 31.90%; ≥90 yrs old: 40.03%. [NOTE: Data at the older ages needs to be interpreted with caution, given the possibility of other causes [e.g. the isolation, the loneliness, inappropriate treatments etc. as reported in numerous other papers, that may have severely impacted the outcome of survival in the elderly. Of course, the abstract results only focus on the older ages!] (Marschner, 2021)
- 0-9 yrs old: 0%; 10-19 yrs old: 0%; 20-29 yrs old: 0.02%; 30-39 yrs old: 0.06%; 40-49 yrs old: 0.04%; 50-59 yrs old: 0.63%; 60-69 yrs old: 2.16%; 70-79 yrs old: 14.41%; 80-89 yrs old: 31.90%; ≥90 yrs old: 40.03%. [NOTE: Data at the older ages needs to be interpreted with caution, given the possibility of other causes [e.g. the isolation, the loneliness, inappropriate treatments etc. as reported in numerous other papers, that may have severely impacted the outcome of survival in the elderly. Of course, the abstract results only focus on the older ages!] (Marschner, 2021)
- “Across all countries, the median IFR in community-dwelling elderly and elderly overall was 2.4% (range 0.3%-7.2%) and 5.5% (range 0.3%-12.1%). IFR was higher with larger proportions of people >85 years. Younger age strata had low IFR values (median 0.0027%, 0.014%, 0.031%, 0.082%, 0.27%, and 0.59%, at 0-19, 20-29, 30-39, 40-49, 50-59, and 60-69 years)…The IFR of COVID-19 in community-dwelling elderly people is lower than previously reported. Very low IFRs were confirmed in the youngest populations.” (Axfors and Ioannidis, 2021)
- “…we estimate the overall IFR [Infection Fatality Rate] in a typical low-income country, with a population structure skewed towards younger individuals, to be 0.23% (0.14-0.42 95% prediction interval range). In contrast, in a typical high income country, with a greater concentration of elderly individuals, we estimate the overall IFR to be 1.15% (0.78-1.79 95% prediction interval range).” (Brazeau et al., 2020)
- “This suggests that the overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.” (Fauci et al., 2020)
- “Infection fatality rates ranged from 0.00% to 1.63%, corrected values from 0.00% to 1.54%. Across 51 locations, the median COVID-19 infection fatality rate was 0.27% (corrected 0.23%): the rate was 0.09% in locations with COVID-19 population mortality rates less than the global average (< 118 deaths/million), 0.20% in locations with 118–500 COVID-19 deaths/million people and 0.57% in locations with > 500 COVID-19 deaths/million people. In people younger than 70 years, infection fatality rates ranged from 0.00% to 0.31% with crude and corrected medians of 0.05%.” (Ioannidis, 2021)
- “Age-specific COVID-19 cases and deaths in Victoria, Australia, during 25 January through 10 December, 2020. Observed case fatality risk (CFR) is the ratio of deaths to cases.” (data in Table 1):
- Recovery rates have been reported as being between 97% and 99.75% (Nikhra, 2020)
- Comorbidity with other diseases (e.g. obesity, heart failure, chronic kidney disease) is a significant contributor to death (Petrilli et al., 2020; Zhou et al., 2020) and makes up ~ 94% of reported deaths (“For 6% of the deaths, COVID-19 was the only cause mentioned”) (CDC, 2020a).
- Comorbidities play a significant role in COVID-19 deaths in children, otherwise the risk of death is low:
- “Results: Mortality in SARS-COV2 infected people varied considerably, between 7 and 155 deaths per million per year in the under-20 age groups compared to 441 to 15,929 in the older age groups. Mortality in pediatric populations is strongly associated with comorbidities (OR: 4.6-47.9) compared to the milder association for older age groups (OR: 3.16–1.23). Conclusion: The risk of death from SARS-COV2 infection in children is low and is strongly associated with comorbidities.” (Gonzalez-Garcia et al., 2021).
- “Children with comorbidities have a higher risk of severe COVID-19 and associated mortality than children without underlying disease.” (Tsankov et al., 2021)
- “Forty patients (83%) had significant preexisting comorbidities…Prehospital comorbidities appear to be an important factor in children.” (Shekerdemian et al., 2020)
- “Results: Mortality in SARS-COV2 infected people varied considerably, between 7 and 155 deaths per million per year in the under-20 age groups compared to 441 to 15,929 in the older age groups. Mortality in pediatric populations is strongly associated with comorbidities (OR: 4.6-47.9) compared to the milder association for older age groups (OR: 3.16–1.23). Conclusion: The risk of death from SARS-COV2 infection in children is low and is strongly associated with comorbidities.” (Gonzalez-Garcia et al., 2021).
- “Among 148,494 adults who received a COVID-19 diagnosis during an emergency department (ED) or inpatient visit at 238 U.S. hospitals during March-December 2020, 28.3% had overweight and 50.8% had obesity. Overweight and obesity were risk factors for invasive mechanical ventilation. Obesity was a risk factor for hospitalization and death, particularly among adults aged <65 years.” (Kompaniyets et al., 2021)
- Reason for link between obesity being a comorbidity in COVID-19-related deaths: “Collectively, our findings indicate that adipose tissue supports SARS-CoV-2 infection and pathogenic inflammation and may explain the link between obesity and severe COVID-19” (Martínez-Colón et al., 2021)
- Percent mortality among COVID-19 patients, April-August 2020:
- No comorbidities: 0-18: 0.00%; 19-29: 0.02%; 30-39: 0.06%; 40-49: 0.14%; 50-59: 0.40%; 60-69: 0.97%; 70+: 2.74% (FAIR Health et al., 2020)
- No comorbidities: 0-18: 0.00%; 19-29: 0.02%; 30-39: 0.06%; 40-49: 0.14%; 50-59: 0.40%; 60-69: 0.97%; 70+: 2.74% (FAIR Health et al., 2020)
- Comorbidities play a significant role in COVID-19 deaths in children, otherwise the risk of death is low:
- Inflammation is a key issue in COVID-19: “Accumulating evidence suggests that severe COVID-19 is associated with an increased plasma level of inflammatory mediators including cytokines and chemokines such as interleukin (IL)-2, IL-6, IL-7, IL-10, tumor necrosis factor alpha (TNF-α), monocyte chemoattractant protein-1 (MCP1; also known as CCL2), macrophage inflammatory protein 1 alpha (MIP1α; also known as CCL3), C-reactive protein, ferritin, and D-dimers (Hojyo et al., 2020).” (Hoertel et al., 2021)
- “Controlling the inflammatory response may be as important as targeting the virus. Therapies inhibiting viral infection and regulation of dysfunctional immune responses may synergize to block pathologies at multiple steps. At the same time, the association between immune dysfunction and outcome of disease severity in patients with COVID-19 should serve as a note of caution in vaccine development and evaluation.” (Tay et al., 2020)
- “Overall, experiments from multiple independent laboratories of the SAVE/NIAID network with several different B.1.1.529 [the Omicron variant] isolates demonstrate attenuated lung disease in rodents, which parallels preliminary human clinical data.” (Diamond et al., 2021)